Every patient is an individual with their own unique circumstances, concerns and expectations. As such Dr Chandra will provide a carefully considered treatment plan tailored for you, the individual. After gathering information from your clinical history, physical examination and investigations he will create an integrated treatment strategy which will centre around lifestyle changes, medications, therapeutic interventions, and onward specialist referral if needed.
Lifestyle advice
– improvements to your lifestyle are important whether you are trying to minimise risk of heart disease or as part of treatment for an established heart condition and focuses on diet, bodyweight, exercise, stress and habits (e.g. smoking). Dr Chandra fundamentally believes in the importance of a healthy lifestyle in staying on top of your heart health.
A balanced diet is important for your health in general and will reduce your risk of high blood pressure, high cholesterol and diabetes. It also prevents obesity and minimises your chance of developing heart disease. Obesity is damaging to your heart and health in general. This is a growing public health concern in the UK and increases blood pressure, cholesterol, the risk of diabetes and the risk of heart disease.
A balanced diet is important for your health in general and will reduce your risk of high blood pressure, high cholesterol and diabetes. It also prevents obesity and minimises your chance of developing heart disease. Obesity is damaging to your heart and health in general. This is a growing public health concern in the UK and increases blood pressure, cholesterol, the risk of diabetes and the risk of heart disease.

Lack of exercise contributes to the risk of developing obesity. The heart is like any muscle and regular exercise helps it work more efficiently. Regular exercise can reduce the risk of heart disease by as much as 35% with an important impact on weight, blood pressure, cholesterol, sugar levels and mood. Stress in your personal or professional life can affect you emotionally and physically and cause changes in behaviour. Recognising and managing stress is important for your health in general and methods to alleviate it include exercise, being outdoors, eating healthily, mindfulness and meditation.
Medications
– there are a variety of medications which prevent heart disease, keep symptoms under control and treat heart conditions. Effective treatment with tablets is a two-way process relying upon your understanding of how to take them safely and your doctor explaining their effects and intended benefits to you. Every medication has the potential to cause side effects, but these are usually temporary and most people do not experience side effects. If a medication makes you feel better, this is a good sign suggesting it is having the desired effect. Please continue taking the medication as your heart condition may deteriorate again if you stop.
If medications are required, Dr Chandra will explain why they are needed, the intended benefits, potential risks and will warn you of any side effects or interactions with other medications. There are several different types of medications (outlined below alphabetically). Please be aware this is not an exhaustive list and some individuals require medications outside this list.
If medications are required, Dr Chandra will explain why they are needed, the intended benefits, potential risks and will warn you of any side effects or interactions with other medications. There are several different types of medications (outlined below alphabetically). Please be aware this is not an exhaustive list and some individuals require medications outside this list.

| Medication | Examples | Method of action | Used to treat |
|---|---|---|---|
| ACE-i | - Ramipril - Perindopril - Lisinopril |
Angiotensin-converting enzyme inhibitor, blocks hormones that allow blood vessels to dilate & take strain off the heart |
- Heart failure - High blood pressure - Coronary artery disease - Kidney problems |
| ARBs | - Candesartan - Losartan - Irbesartan |
Angiotensin II receptor blocker, blocks hormones that allow blood vessels to dilate & take strain off the heart |
- Heart failure - High blood pressure - Coronary artery disease - Kidney problems |
| Antiarrhythmics | - Amiodarone - Flecainide |
Act on electrical channels in the heart to control conduction |
- Heart rhythm disturbance - Maintain normal rhythm |
| Anticoagulants | - Warfarin - Apixaban - Rivaroxaban |
Blood thinners that affect blood clotting system to prevent clot formation and stroke |
- Atrial fibrillation - LV thrombus - Mitral valve disease |
| Antiplatelets | - Aspirin - Clopidogrel - Ticagrelor |
Act on receptor on platelets in the blood to prevent them sticking together |
- Coronary artery disease - After PCI & coronary stents - Stroke |
| Beta-blockers | - Bisoprolol - Nebivolol - Sotalol |
Block receptors in the heart to slow the heart rate, reduce the blood pressure & take strain off the heart |
- Coronary artery disease - Heart failure - High blood pressure - Atrial fibrillation |
| Calcium channel blockers | - Amlodipine - Diltiazem |
Block receptors in the heart to slow the heart rate, reduce the blood pressure & take strain off the heart |
- Coronary artery disease - High blood pressure - Atrial fibrillation |
| Cholesterol lowering drugs | - Atorvastatin - Rosuvastatin - Ezetimibe |
Inhibits enzymes involved in metabolism of cholesterol & reduces LDL (bad) cholesterol |
- High cholesterol - Coronary artery disease - Stroke |
| Diuretics | - Frusemide - Bumetanide - Bendrofluazide |
Work in the kidneys to remove excess fluid & take the strain off the heart |
- Heart failure - High blood pressure |
| Nitrates | - GTN - ISMN |
Relax the blood vessels causing them to dilate. Improves blood supply to the heart & reduces blood pressure |
- Angina - High blood pressure - Heart failure |
| Miscellaneous | - Nicorandil - Ranolazine - Ivabradine |
Work in different parts of the heart to improve blood supply to the heart musce and/or take stain off the heart |
- Coronary artery disease - Angina - Heart failure |
Therapeutic Interventions
Beyond lifestyle changes and medications there are a number of therapeutic interventions that may be necessary to treat heart disease. Examples that Dr Chandra provide include DC cardioversion, permanent pacemaker implantation, percutaneous coronary intervention and intervention for structural heart disease.
Beyond lifestyle changes and medications there are a number of therapeutic interventions that may be necessary to treat heart disease. Examples that Dr Chandra provide include DC cardioversion, permanent pacemaker implantation, percutaneous coronary intervention and intervention for structural heart disease.
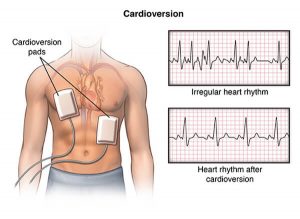
- DC Cardioversion (DCCV) – is considered for patients with arrhythmia where the aim is to use electrical therapy to the heart to restore normal heart rhythm. Most commonly this is performed for people with atrial fibrillation or atrial flutter. DCCV usually requires a short stay in hospital (4-6hrs). You will be connected to an ECG and blood pressure monitor throughout the procedure and given either sedation or a short general anaesthetic. Defibrillator pads are attached to your chest and one or more controlled electrical shocks are given to the heart to restore normal rhythm. Afterwards, we will monitor your heart rate, rhythm and blood pressure and Dr Chandra advise on any changes to your medications.
- Permanent pacemaker (PPM) implantation – the heart has a natural pacemaker, the ‘sinus node’ that sends out regular electrical impulses causing the chambers of the heart to contract and produce a heartbeat. If the sinus node or the electrical pathways do not work properly you may need a PPM. This small device (the size of a matchbox) sends electrical impulses to keep your heartbeat regular. A PPM is also used to treat arrhythmia, particularly where the heartbeat is either too slow, missing beats, or beating too fast but uncontrolled effectively with medication. PPM implantation is a sterile procedure performed under local anaesthetic and sedation that typically takes 60 minutes. It is usually implanted under the collar bone on the left side with one or two wires (leads) running directly to the heart. You will have a scar of ∼5cm in length under the collar bone. It is a day-case procedure and you will go home on the same day after a few hours of monitoring. If you need a PPM, Dr Chandra will explain the intended benefits and potential risks and perform the procedure himself.

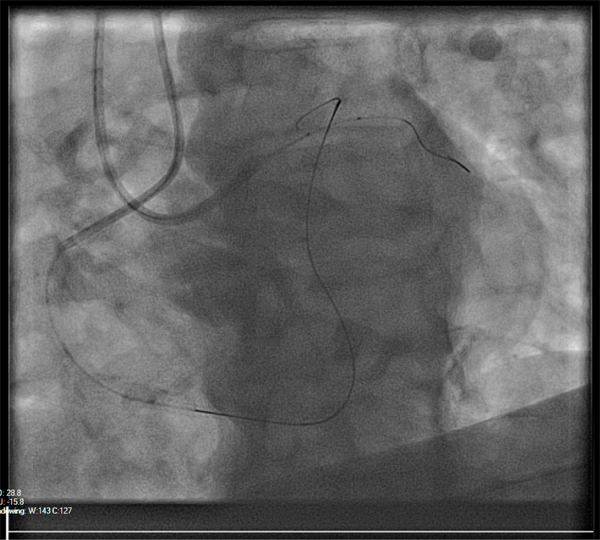
- Percutaneous Coronary Intervention (PCI) – also known as coronary angioplasty, is a treatment designed to improve the blood supply to the heart muscle. In some individuals the coronary arteries become narrowed and furred up with fatty deposits called atheroma which compromises blood flow. This may lead to symptoms of chest pain or breathlessness particularly with exertion, called angina. Coronary atheroma can be picked up on a 12-lead ECG, exercise stress testing, CT coronary angiography or invasive coronary angiography. PCI is widely used as an emergency treatment for heart attacks and also to relieve symptoms of angina by widening the narrowed or blocked arteries to allow the return of normal blood flow.
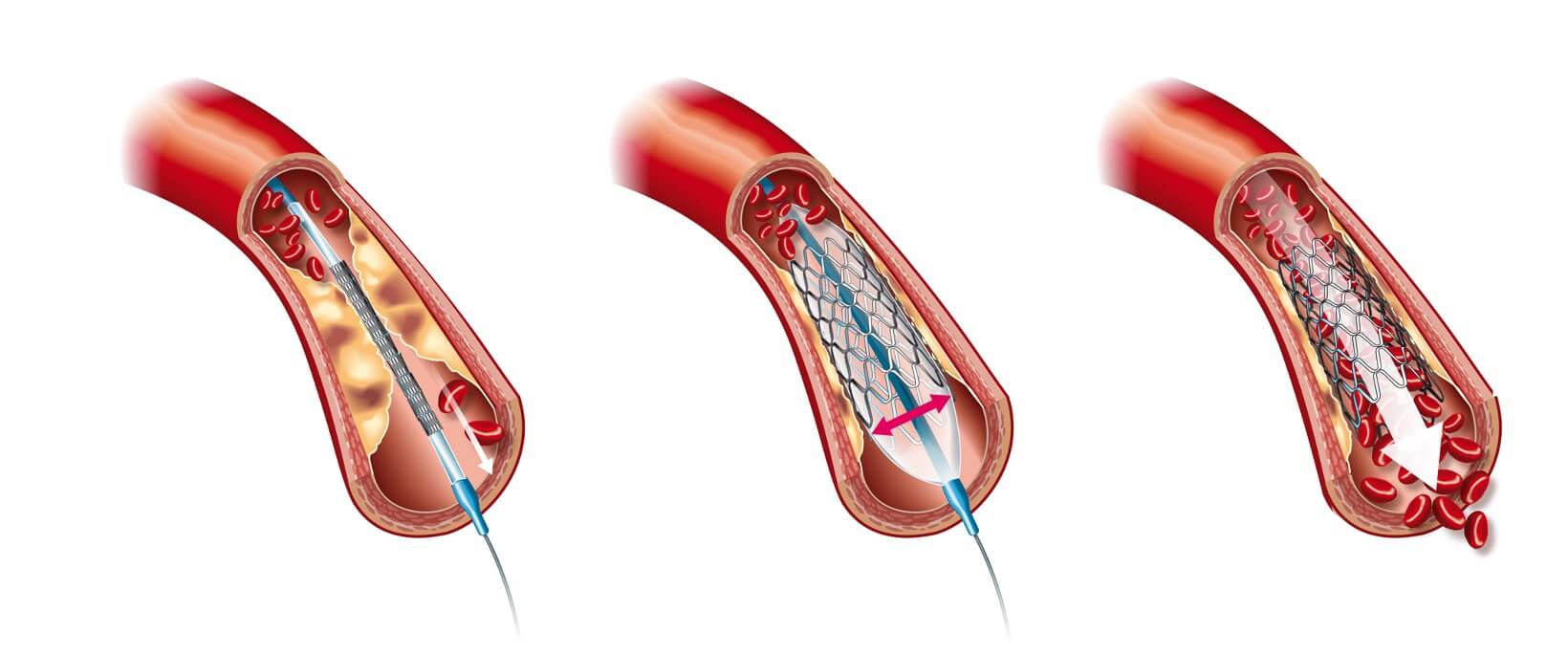
- A coronary angiogram is performed prior to PCI (typically from the radial artery at the wrist). After a local anaesthetic injection at the wrist, a small plastic tube (sheath) is placed into the radial artery. From here catheters are passed to the heart and special dye injected directly into the coronary arteries. This will identify where the narrowings and/or blockages within the coronary arteries are located. Once the decision to perform PCI has been made we will pass a special guide-wire into the coronary artery and through the narrowed/blocked segment. We use this wire to deliver equipment into the coronary artery. Initially a balloon is delivered and inflated to open up the narrowed/blocked vessel. Then a coronary stent (stainless steel scaffold) is delivered into the diseased segment and deployed into the coronary artery. Finally a stiffer balloon is passed inside the stent and inflated to ensure the stent has achieved its maximal size and is fully lining the coronary artery. The stents are coated with special drugs to minimise the chance of future problems in the same area. When the procedure is complete, the equipment is removed leaving only the stent in the coronary artery behind. You will be monitored for 4 hours to ensure the heart rate, heart rhythm and blood pressure are within safe limits and you will go home on the same day. If you need PCI, Dr Chandra will explain the intended benefits and potential risks and will perform the procedure personally.
- Precision PCI – with the experience gained from his international Fellowship in Canada, Dr Chandra specialises in ‘precision PCI’. This incorporates ‘state-of-the-art’ adjunctive technology in your procedure to ensure the best outcomes for you. In essence, this involves evaluating the coronary artery (and any atheroma) and creating a tailored PCI strategy that is unique to you and relies on evidence-based techniques including:
Optical Coherence Tomography (OCT)
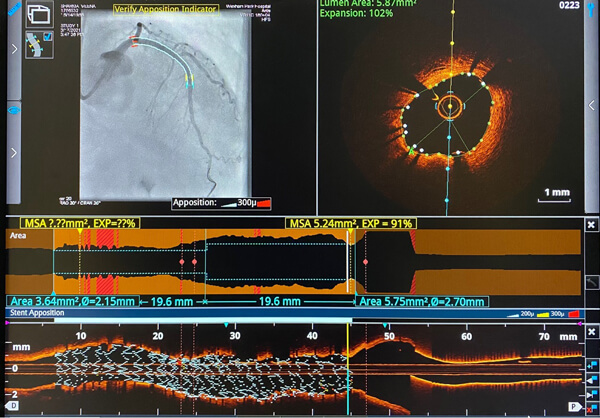
It is a different form of imaging the inside of the coronary artery using light waves to generate highly detailed anatomical pictures. This also involves passing a small microcatheter into the coronary artery that has a specialised light probe at the tip. This facilitates detailed characterization of any atheroma (e.g. clot, calcification, fatty tissue), assessment of the coronary artery architecture and allows for highly accurate sizing of the vessel. Once treated with stents the coronary artery can be re-evaluated with OCT to ensure excellent results.
Intravascular ultrasound (IVUS)

IVUS is a form imaging the inside of the coronary artery using ultrasound waves to generate a moving picture of the vessel and any atheroma. This involves passing a small microcatheter into the coronary artery that has a specialised ultrasound probe at the tip. Once the images of the coronary artery are obtained we can characterise the atheroma and size the area requiring treatment accurately from inside the vessel. Once treated with stents, the coronary artery can be re-evaluated with IVUS to ensure excellent results.
Pressure wire study (PWS)
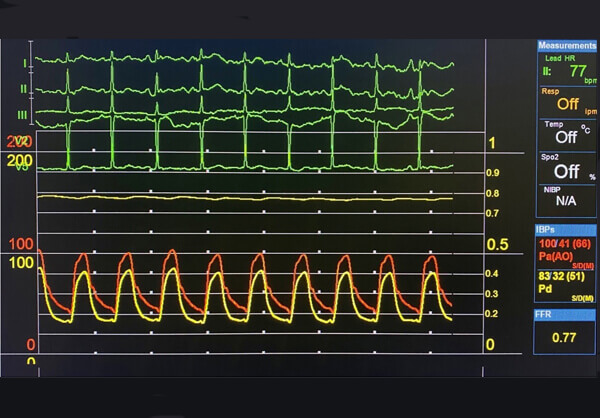
PWS is based upon the principle of assessing the blood flow in the coronary artery and assessing if it is truly affected by an area of atheroma in the vessel. This can help us to understand whether a stent is required to improve blood flow to the heart muscle and if there will be clinical improvement as a result. This involved passing a sensor into the coronary artery and measuring blood flow before the narrowing and then beyond the narrowing. A drug called adenosine is used to help gather this information. If blood flow is compromised a stent will be placed as outlined above and the flow measured again to confirm improvement.
-
Complex & High-risk PCI (CHIP) – unfortunately, some patients have high-risk or complex coronary artery disease. This can be due to individual patient factors, other health problems or specific technical challenges of the coronary artery itself. Often this involves patients with longstanding chronically occluded coronary arteries (CTO), those with hardened and heavily calcified coronary arteries or those with multiple coronary artery disease that are unsafe or unfit for heart surgery. Performing PCI in such individuals requires careful planning, risk assessment and technical skill. Such procedures often take longer to perform, require more specialist equipment and warrant an overnight stay in hospital for closer monitoring. With his extensive experience in advanced coronary intervention, Dr Chandra specialises in complex and high-risk PCI cases and often performs these as joint cases with his colleague and friend Dr Joshua Chai.
Together, they have established a ‘CHIP’ program at Wexham Park Hospital so that patients with all forms of coronary artery disease can be treated safely and effectively. They regularly perform successful PCI for patients with ‘left main stem disease’, ‘chronic total occlusions (CTO)’ and have acquired specialised equipment to facilitate PCI for heavily calcified coronary arteries, including RotaPro & Shockwave.
- Intervention for Structural Heart Disease – this is a growing area of Cardiology as there are increasing needs for patients with heart valve disease who are deemed too high risk for conventional heart surgery. Most commonly, this is for individuals with a severely narrowed aortic valve, known as aortic stenosis. With time the aortic valve can become hardened, stiff and calcified. The valve does not open fully and this makes it harder for the heart to pump blood through the valve and around the body leading to symptoms of breathlessness, fatigue and dizziness.
Previously the only treatment option was open heart surgery to replace the aortic valve. This remains an excellent treatment for severe aortic stenosis but is not suitable for all patients.
Transcatheter aortic valve implantation (TAVI) does not require open heart surgery and is a form of ‘keyhole’ aortic valve replacement performed using catheters via the larger arteries in the leg. Initially TAVI was used for patients that were considered too high risk for aortic valve surgery. However, there is increasing clinical evidence to suggest that this is a safe and effective alternative to heart surgery in a growing population of patients with aortic stenosis.
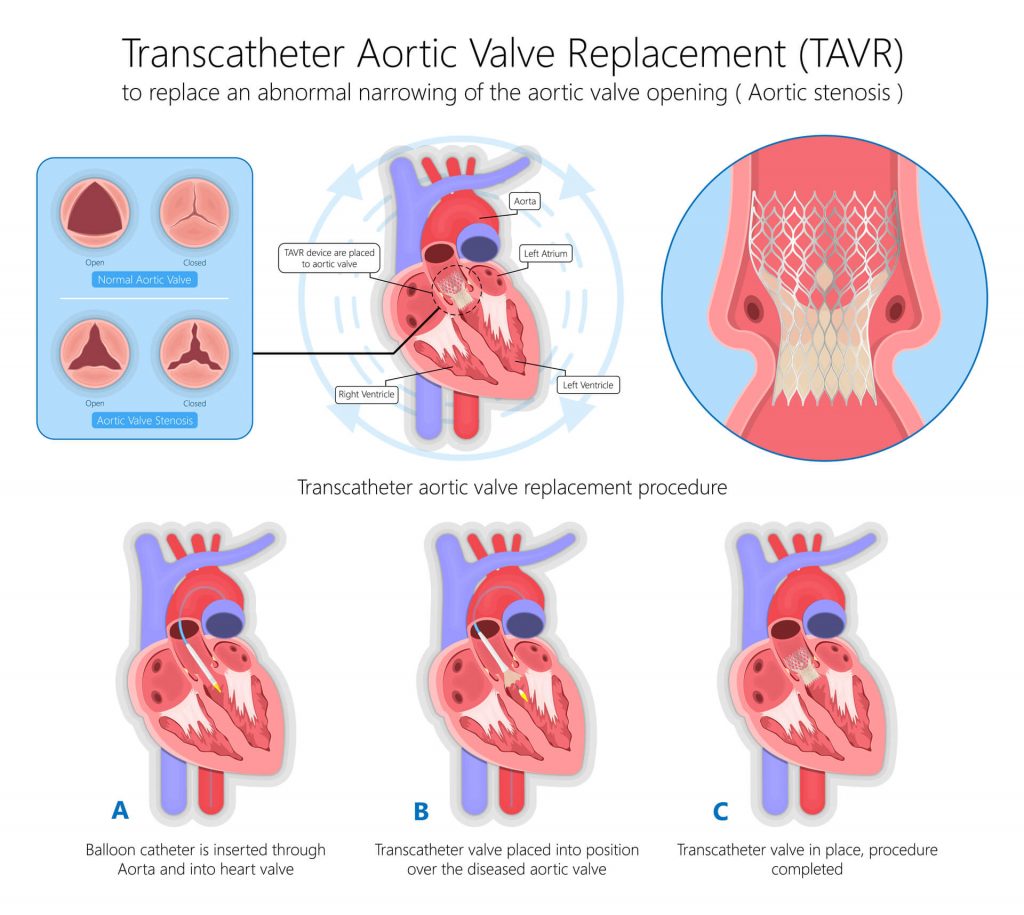
- Dr Chandra is part of the structural heart disease team at Harefield Hospital (Royal Brompton & Harefield NHS Foundation Trust) managing patients with severe aortic stenosis that require TAVI. He has a close working relationship with the Interventional Cardiologists, Cardiothoracic surgeons, Radiologists and specialist nurses to ensure excellent outcomes for patients requiring this procedure. If you have structural heart disease, Dr Chandra will ensure that you receive the most appropriate treatment via this network.
- Onward Specialist Referral – once you have been evaluated by Dr Chandra and a diagnosis reached, you may require onward specialist referral for a definitive management strategy. This may be the case if you have advanced heart failure requiring cardiac device therapy (CRT-P or CRT-D), arrhythmia requiring electrophysiological study and ablation, or severe coronary artery disease and/or heart valve disease requiring open heart surgery. Dr Chandra has an extensive network of specialist colleagues that have a wealth of experience in these specific areas and will ensure swift onward referral when required.
After careful evaluation, if a cardiac cause of your symptoms is not identified Dr Chandra will happily refer you to physicians with expertise in other medical specialties when needed.

- For example, this may include Respiratory physicians for further evaluation of breathlessness, Gastroenterology or Rheumatology for chest discomfort, Endocrinology for hormonal causes of palpitations, or Neurology for dizziness with blackouts without a cardiac cause.
If after seeing Dr Chandra you would like a second opinion, he will be more than happy to recommend another Cardiologist and welcomes any feedback that you may have to improve his service or your experience.

